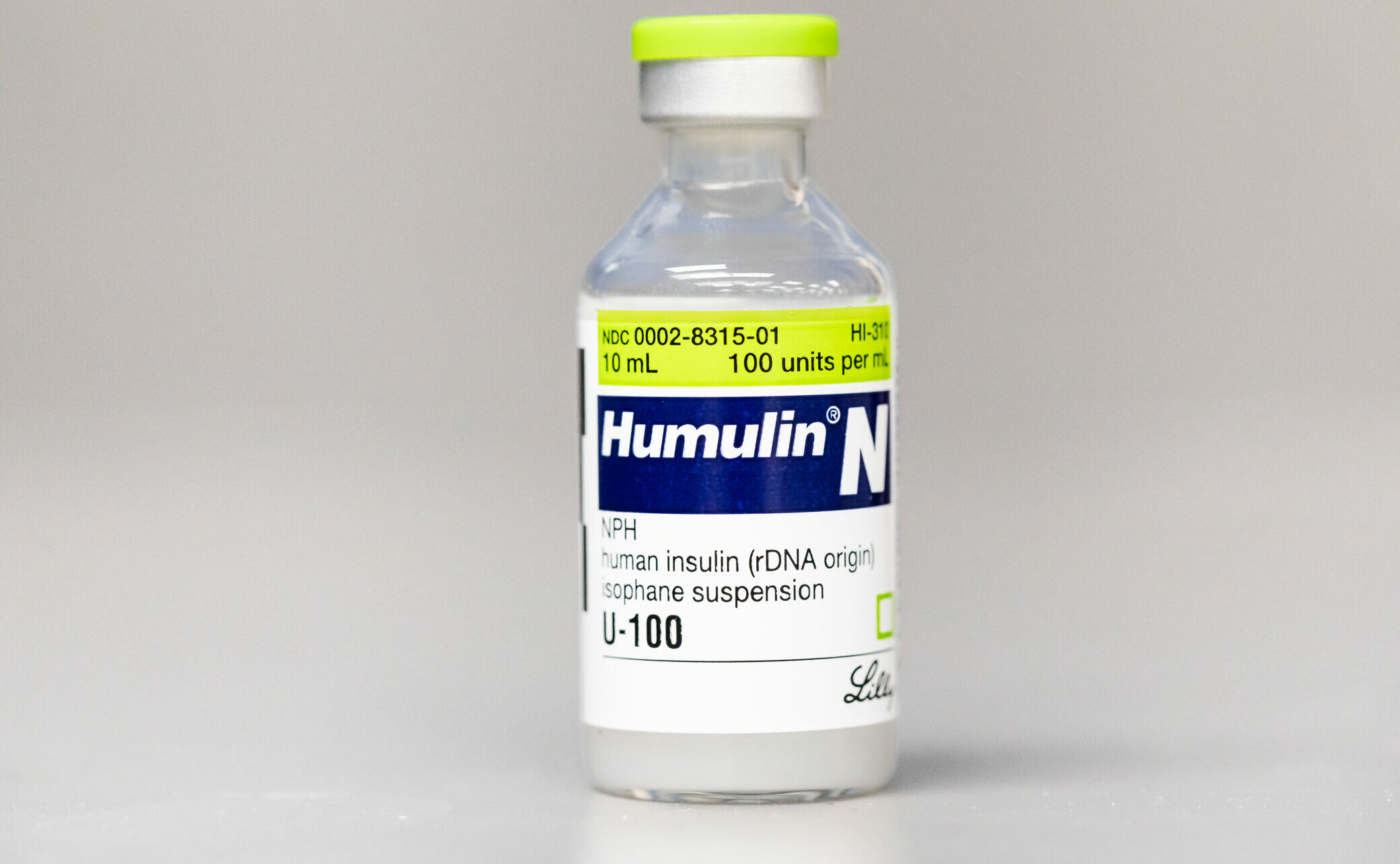
Humulin is one of Eli Lilly’s most common synthesized insulin products. Photo by Lauren Gdowski.
ZOE MILLER | STAFF REPORTER | zjmiller@butler.edu
Eli Lilly and Company recently announced that the out-of-pocket cost of insulin would be capped at $35 or less for patients who qualify for the Lilly Insulin Value Program. The list price of Humalog and Humulin, two of the most common types of insulin sold by Eli Lilly, will also be cut by 70% in the near future for all insulin users. Eli Lilly is one of the first pharmaceutical companies to enact policies that will dramatically decrease the cost of insulin.
The 70% price cut on Humalin and Humalog is available for all insulin users. However, only patients eligible for the Insulin Value Program are guaranteed to receive insulin for an out-of-pocket price of $35 or less. Eligibility for the program requires a patient to have commercial drug insurance or no insurance, and no access to other discounts on Lilly insulin.
Dr. Andrew Schmelz is an assistant professor of pharmacy at Butler and the faculty director of diversity, equity and inclusion for the Butler College of Pharmacy and Health Sciences. Schemlz said that unlike many other medications, insulin is very expensive to produce.
This is due to the fact that insulin produced by pharmaceutical companies is synthetic, replicating what is naturally produced in the human body. Synthetic insulin can also be manufactured to last longer and absorb more quickly in the body, making it much more effective. As insulin products are continually under patent, it is not possible to manufacture generic insulin, which would result in cheaper production costs. Because of this, insulin prices remain high.
“What is kind of unfortunate is that we’re still talking about [older products] that probably don’t work quite as well as some of our newer options,” Schmelz said.
The recent policy announced by Lilly will affect the price of older products that are less advanced than newer treatments for diabetes such as non-insulin treatments for type 2 diabetes, like Trulicity. Newer products at Lilly can be more effective in the treatment of diabetes, but will not be included in the price cut. While older products such as Humalog and Humulin can effectively treat diabetes, newer products work in more advanced ways.
Along with working at Butler, Schmelz also works at Eskenazi Health. He works directly with patients who don’t have insurance and are not able to easily access medication. The price cut on insulin products is beneficial for patients without insurance because they will have access to a more affordable option. However, patients that require the use of newer products such as Trulicity will still be required to pay much more.
“The [medication] I would like to use for patients is … still probably going to be more expensive,” Schmelz said.
While the price cap makes older insulin products more affordable, Lilly has many newer products that are earning the company a significant amount of profit.
“It’s really coincidental that Lilly in particular [is making this decision when] they have new products for diabetes that are super expensive, [and] are generating a lot of money for them right now,” Schmelz said. “That’s how they’re probably justifying doing this … It’s not really going to hurt [them] that much.”
Prior to Lilly’s announcement, Congress passed the Inflation Reduction Act in August of 2022. This act specifically caps the out-of-pocket price of all insulin products at $35 for seniors with Medicare.
Samantha Plumridge, a sophomore strategic communication major, was diagnosed with type 1 diabetes when she was five years old. She uses insulin every hour of the day through a medical pump that is always connected to her body. Plumridge said type 1 diabetes stems from issues within the pancreas and its inability to produce the required amount of insulin to survive.
“My pump is my pancreas,” Plumridge said. “It is what gives me insulin.”
Without access to insulin, Plumridge said that her body’s blood sugar would spike, and she would be hospitalized at the risk of death. While she has been fortunate enough to always have access to the insulin she needs, this is not the case for everyone. Many diabetic individuals do not have sufficient funds or proper access to the insulin they need to survive. This is the obstacle that Eli Lilly is trying to solve by capping the out-of-pocket cost.
Cate Pugliese, a first-year sociology-criminology major, was diagnosed with type 1 diabetes when she was six. She uses insulin every three days. Pugliese said that while her family is able to afford insulin, it is still very expensive considering she needs it to survive.
“Usually it’s like $300 … with insurance,” Pugliese said. “It was like $20 [after the announcement], and [my mom] was so happy about it.”
Pugliese said that her family has to purchase insulin every three months. Even for families like hers that are able to afford insulin, a reduction in the price is still beneficial and will relieve financial stress.
Eli Lilly stated in the press release for the price cap that the new policy was a call to action for other companies as well. Novo Nordisk, another supplier of insulin in the United States, announced a price cut on insulin shortly after. Lilly is one of only three insulin suppliers in the country. In the United States, three out of 10 insulin users use insulin from Lilly. In order to ensure all users have easy access to insulin, all three companies would need to initiate a change in the affordability of their products.
“We still have a lot of ground to cover in terms of helping people afford medications in general,” Schmelz said.



Pingback: Insulin accessibility | The Butler Collegian - technewscomboho.in